Abstract
Multiple myeloma is the second most frequent hematological malignancy in the world. It is characterized by bony destruction, anemia, worsening renal function, and immune system compromise, which makes it an aggressive and limiting disease with high morbidity and mortality. To optimize outcomes and patients' quality of life it is necessary to achieve adequate control of the disease by improving adherence to treatment and reinforcing patient education. The objective of our study is to measure the impact of a new education strategy based on digital, personalized, spaced-learning, on treatment adherence, adverse effects prevention, and quality of life of multiple myeloma patients.
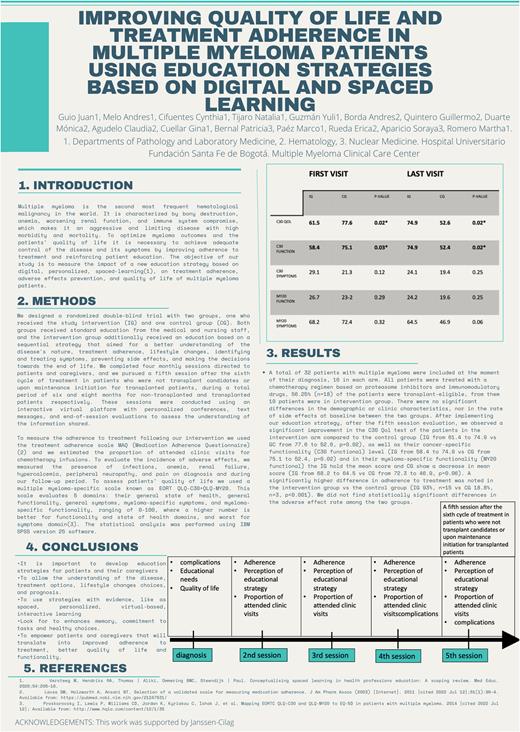
We designed a randomized double-blind trial with two groups, one who received the study intervention (IG) and one control group (CG). Both groups received standard education from the medical and nursing staff, and the intervention group additionally received an education based on a sequential strategy that aimed for a better understanding of the disease's nature, treatment adherence, lifestyle changes, identifying and treating symptoms, preventing side effects, and making the decisions towards the end of life. We completed four monthly sessions directed to patients and caregivers, and we pursued a fifth session after the sixth cycle of treatment in patients who were not transplant candidates or upon maintenance initiation for transplanted patients, during a total period of six and eight months for non-transplanted and transplanted patients respectively. These sessions were conducted using an interactive virtual platform with personalized conferences, text messages, and end-of-session evaluations to assess the understanding of the information shared.
To measure the adherence to treatment following our intervention we used the treatment adherence scale MAQ (Medication Adherence Questionnaire) and we estimated the proportion of attended clinic visits for chemotherapy infusions. To evaluate the incidence of adverse effects, we measured the presence of infections, anemia, renal failure, hypercalcemia, peripheral neuropathy, and pain on diagnosis and during our follow-up period. To assess patients' quality of life we used a multiple myeloma-specific scale known as EORT QLQ-C30+QLQ-MY20. This scale evaluates 5 domains: general state of health, general functionality, general symptoms, myeloma-specific symptoms, and myeloma-specific functionality, ranging of 0-100, where a higher number is better for functionality and state of health domains, and worst for symptoms domain. The statistical analysis was performed using IBM SPSS version 25 software.
A total of 32 patients with multiple myeloma were included at the moment of their diagnosis, 16 in each arm. All patients were treated with a chemotherapy regimen based on proteasome inhibitors and immunomodulatory drugs, 56.25% (n=18) of the patients were transplant-eligible, from them 10 patients were in intervention group. There were no significant differences in the demographic or clinic characteristics, nor in the rate of side effects at baseline between the two groups. After the fifth session evaluation, we observed a significant improvement in the C30 Qol test of the patients in the intervention arm compared to the control group (IG from 61.4 to 74.9 vs GC from 77.6 to 52.6, p=0.02), as well as their cancer-specific functionality (C30 functional) level (IG from 58.4 to 74.9 vs CG from 75.1 to 52.4, p=0.02) and in their myeloma-specific functionality (MY20 functional) the IG hold the mean score and CG show a decrease in mean score (IG from 68.2 to 64.5 vs CG from 72.3 to 46.9, p=0.06). A significantly higher difference in adherence to treatment was noted in the intervention group vs the control group (IG 93%, n=15 vs CG 18.8%, n=3, p<0.001). We did not find statistically significant differences in the adverse effect rate among the two groups.
In conclusion, it is important that multiple myeloma care programs develop education strategies for patients and their caregivers that allow understanding of the disease, treatment options, lifestyle changes choices, and prognosis, by using spaced, personalized, virtual-based, interactive learning that enhances memory, commitment to tasks and healthy choices, which will empower patients and caregivers and will translate into improved adherence to treatment, better quality of life and functionality.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal